The Mystery and the Misery of Leaky Gut Syndrome

In medical circles, controversy surrounds what the media and many alternative health practitioners call ‘leaky gut syndrome’. Dr Ng Tay Meng, Consultant Gastroenterologist, Ng Tay Meng Gastrointestinal Hepatology Centre, provides a professional opinion.
WHAT IS LEAKY GUT SYNDROME?
“Leaky gut syndrome (LGS), also known as hyper permeable gut or dysfunctional gut barrier, is not a disease by itself but rather a relatively recent concept used to explain the pathogenesis, or origins and development, of some gastrointestinal and extra-gastrointestinal diseases,” shared Dr Ng.
While a growing body of evidence suggests that LGS plays an important role in many chronic diseases, the question of whether it is the cause or effect of these diseases has yet to be answered.
THE ROLE OF THE INTESTINAL BARRIER
To understand LGS, it is essential to grasp a basic understanding of the role of the gut’s intestinal barrier.
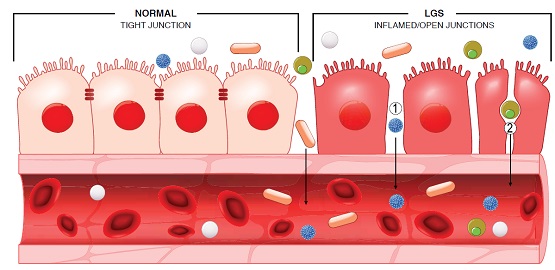
The human body is protected from external harmful factors such as bacteria, viruses, toxin and chemicals by the intestinal barrier. This semi-permeable barrier allows the absorption of food and nutrients, but at the same time prevents the entry of harmful agents into the bloodstream and body.
The intestinal barrier is not just a physical barrier but a functional immunological one as well. It consists of four components – a protective mucus layer, a cellular layer with tight junctions, gut bacterial flora, and immune components of cytokines and immune cells. The integrity of the barrier requires the dynamic and symbiotic interaction of these components.
Any factors that disrupt the integrity of any of these components can make the barrier become more ‘porous’ or defective, allowing the passage of harmful bacteria, viruses, toxins and chemicals into our bloodstreams and tissues.
“The presence of these harmful agents will then trigger an immune response from the body’s immune system, creating antibodies and immune cells to destroy them. Chronic overstimulation of the immune system will lead to chronic inflammation in the body or organs, resulting in diseases,” said Dr Ng.
WHAT ARE THE SYMPTOMS?
According to Dr Ng, the symptoms associated with LGS are numerous, and vary depending on the disease or organs affected.
If the organ affected is the gut, LGS may cause gastrointestinal symptoms such as chronic diarrhoea, constipation, flatulence, abdominal pain or bloating and nutritional deficiency, which also occurs in patients with irritable bowel syndrome, inflammatory bowel disease or celiac disease.
If other organs such as the skin, brain, nerves, and joints are affected, symptoms such as headache, chronic fatigue syndrome, body ache and pain, skin rash, acne or eczema and joint pain can occur.
WHAT ARE THE UNDERLYING CAUSES?
A number of gastrointestinal conditions, such as inflammatory bowel disease, irritable bowel syndrome, celiac disease and food allergies, are known to be associated with LGS.
Though conclusive data is lacking, scientists also suspect that LGS plays a role in metabolic or systemic diseases such as diabetes mellitus, cardiovascular disease, autoimmune disease, autism, fibromyalgia, dementia, multiple sclerosis, obesity, skin disease and chronic fatigue syndrome.
WHO IS AT RISK?
Aside from genetic factors, the following factors increase the risk of developing LGS.
Diet – An excessive intake of carbohydrates and sugar, especially fructose, can impair the intestine’s barrier function. Certain food additives or preservatives such as emulsifiers have also been shown to deplete the protective mucus layer of the barrier making it defective. Nutritional deficiencies, especially in Vitamins A and D and Zinc, may also contribute to LGS.
Lifestyle – Heavy alcohol consumption, smoking, chronic stress and inadequate rest may also affect the gut health and contribute to LGS.
Drugs – The indiscriminate use of antibiotics and painkillers, especially the nonsteroidal anti-inflammatory drugs (NSAIDS) and proton pump inhibitors, can alter normal gut microbiota and disrupt the integrity of the gut barrier.
Critical illness – Patients who have undergone major abdominal surgery, patients on chemotherapy, trauma patients, burn patients and other intensive care unit patients also have a high risk of LGS due to a combination of factors such bacterial infection and hypo perfusion (reduced blood flow) of the gut.
HOW IS IT DIAGNOSED?
The tests used to diagnose the root cause of LGS depend on the associated disease suspected. For example, for inflammatory bowel disease or celiac disease, blood tests and a gastrointestinal endoscopy are often required. If small bowel bacterial overgrowth is suspected, then a simple breath test can be used for the diagnosis.
HOW IS IT TREATED?
Just as the method of diagnosis depends on the disease suspected, so does the treatment. For instance, if celiac disease is present then a gluten-free diet is mandatory and the gut will become normal after gluten avoidance. If the LGS is linked to inflammatory bowel disease, then specific therapy with immunosuppressive drugs will be required.
WHAT ARE THE POSSIBLE COMPLICATIONS?
If the underlying conditions associated with LGS are not diagnosed and addressed, serious complications can occur. For example, untreated LGS can lead to malabsorption of important nutrients and vitamins, intestinal stricture and perforation.
“The worst-case scenario is bacterial translocation into the blood stream from the defective intestinal barrier, causing sepsis and even multi-organ failure and death. The risk of intestinal cancer will also be increased if the disease is not controlled,” explained Dr Ng.
HOW CAN IT BE PREVENTED OR MANAGED?
The good news is, LGS can be prevented or managed with healthy lifestyle choices.
“Certain lifestyle changes such as regular exercise, getting enough sleep every night and reducing stress can improve digestion and support a healthy gut,” advised Dr Ng. “Dietary changes such as reducing refined carbohydrate and high fat intakes and eating less processed food will greatly benefit the gut barrier.”
In particular, Dr Ng recommended choosing high-fibre foods that can boost the good bacteria in our gut flora, such as fruits, vegetables and legumes, and fermented foods such as plain yoghurt, kimchi and kombucha, which contain gut-friendly bacteria.
Dr Ng also advises against the long-term use of NSAIDS (non-steroidal antiinflammatory drugs, which include most over-the-counter painkillers), proton pump inhibitors and antibiotics, all of which can affect the bacteria flora and increase gut permeability.
Very early in life, a mother can give her child the gift of gut health by breastfeeding.
“Breastfeeding has been shown to improve gut health and reduce the risk of gastrointestinal infections and allergies in infants. The colostrum in the breast milk contains immune cells and growth factors that help to stimulate the growth of intestinal cells and heal any intestinal barrier damage, thus preventing intestinal hyperpermeability,” explained Dr Ng.
WHAT NEXT?
“LGS is an exciting growing area for research, as it provides new targets for disease prevention and novel drug therapy for many chronic debilitative diseases for which we still do not have optimal drug therapy,” said Dr Ng.
Faecal transplants, which aim to manipulate and modify the bacteria microbiota in certain diseases such as obesity, inflammatory bowel disease and refractory Clostridium difficile colitis, are showing promising results.
Research continues on the use of probiotics and dietary modifications in the treatment of obesity and metabolic conditions such as diabetes mellitus and fatty liver disease.
“It is possible that one day we will be able to prevent or treat most chronic diseases by modifying what we eat and manipulating our gut microbiota,” suggested Dr Ng. “When Hippocrates said that all disease begins in the gut, he was far ahead of his time.”
You heard it from Dr Ng and Hippocrates. Give your gut the respect it deserves and you could give countless diseases the slip.
Article contributed by Dr Ng Tay Meng, an accredited doctor of Mount Alvernia Hospital.
Ng Tay Meng Gastrointestinal Hepatology Centre
Mount Alvernia Hospital Medical Centre A #06-01
Tel: 6256 0417
This article is taken from our My Alvernia Magazine Issue #41. Click here to read the issue on our website or on Magzter.