
Dr Piotr Chlebicki, Infectious Diseases Specialist at Infectious Diseases Medical Clinic, addresses common questions and concerns about the vaccines that have been approved for use in Singapore.
Q: What is your professional opinion on the vaccines approved for use in Singapore’s COVID-19 Vaccination Programme, the Pfizer-BioNTech vaccine and the Moderna vaccine?
A:Both of these vaccines have been proven effective not only in clinical trials but also in real life. In clinical trials, the effectiveness of the Pfizer vaccine was 94 percent. In the real-life experience in Israel, where around 70 percent of the population has been vaccinated, it is also very positive. I have had the Pfizer vaccine myself, and I think it is a very good vaccine. In fact, it has exceeded expectations. (See ‘The Israel Experience’.)
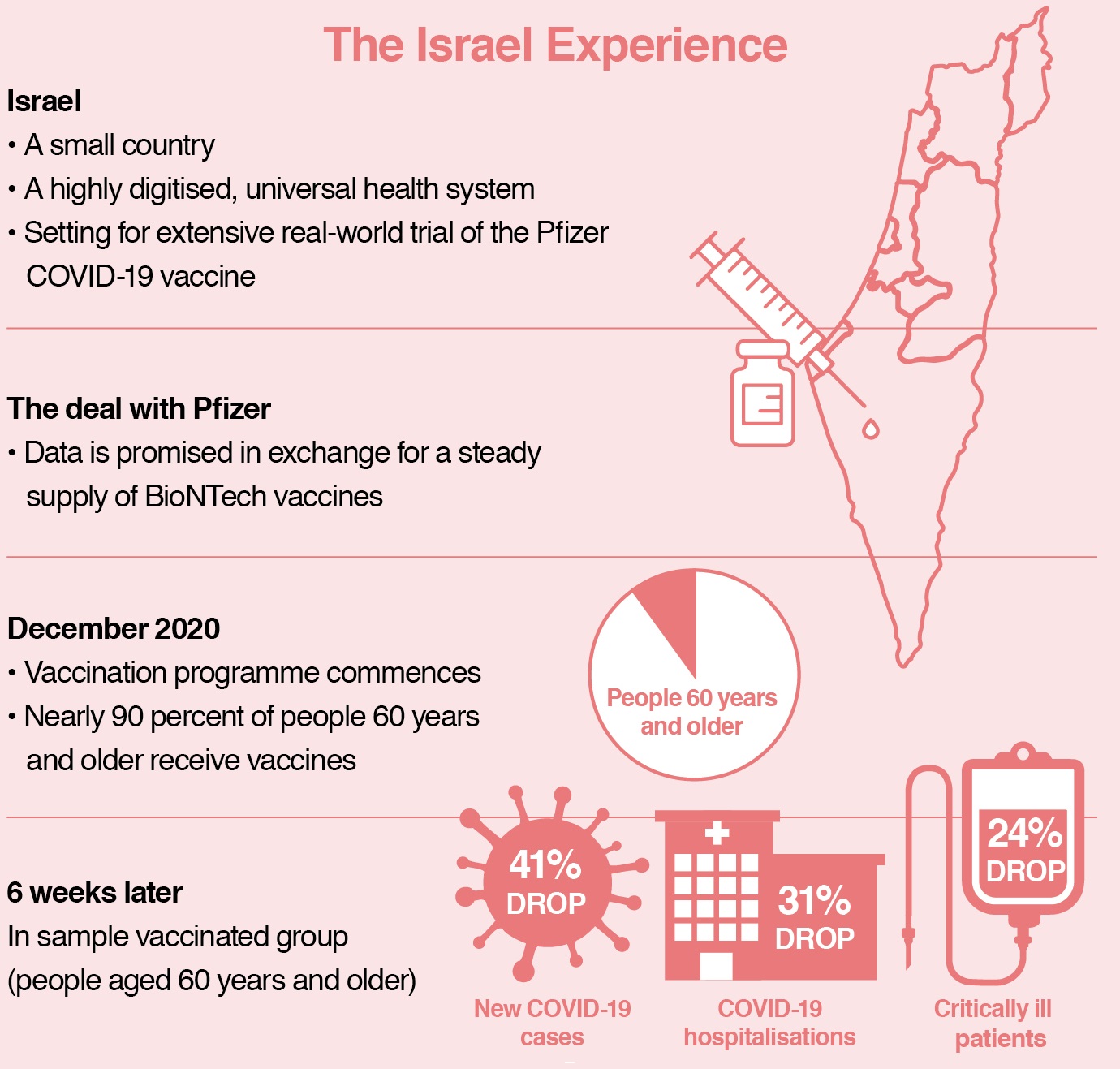
NOTE: In early February, Clalit, Israel’s largest healthcare provider, reported a 94 percent drop in symptomatic COVID-19 cases among 600,000 people who had received two doses of the Pfizer vaccine. This is aligned with the 94 percent effectiveness found during clinical trials of the vaccine.
Q: Why are the vaccines administered in two doses – 21 days apart for the Pfizer vaccine and 28 days apart for the Moderna vaccine?
A:The first dose is to prime the immune system. The second dose is sort of like a reminder. When the immune system learns how to fight the virus, the second dose is an enhancer or booster dose.
Q: The Ministry of Health website warns that severe allergic reactions, including “eye, mouth, or facial swelling, difficulty in breathing and/or a fall in blood pressure” may take place after receiving the vaccine. How common are these allergic reactions?
A:This describes a severe allergic reaction to almost anything. The risk is present with all vaccines, but it is a question of frequency. In clinical trials, the risk of severe allergic reactions was 1 in 100,000 for the Pfizer vaccine, so it is very infrequent. This number comes from one week of reporting from the US in the second half of December. Very soon we will have data based on several weeks of reporting. My guess is that the frequency of severe allergic reactions will be shown to be even lower than that already low number.
Q: If a person has had and recovered from COVID-19, are they considered immune?
A:This is a controversial topic. Initially, for the first several months after infection, the vast majority of patients appear to have very good immunity. However, data shows that after some time, in some people, the antibody level drops. More time, and more data, will tell us more.
Q: Should people who have had COVID-19 be vaccinated?
A:It depends on the geographical perspective. In countries where the pandemic is raging, it does not make sense logistically to check who has and has not had COVID-19. Whether it is really helpful is open for debate. I think the compromise may be to give these people one dose instead of two doses, to boost their own antibodies.
Q: If a person has had COVID-19 and is then vaccinated, would they have a higher than normal risk of suffering serious side effects after receiving the vaccine?
A:Initially, with other vaccines a previous infection can increase the risk of serious side effects. But so far, this does not seem to apply to the approved COVID-19 vaccines.
Q: Why do the approved vaccines not work in a small percentage of people?
A:There are a few reasons. There is a small proportion of people who just do not respond to vaccines. These are usually people with certain medical conditions, with severely weakened immune systems that are unable to mount an appropriate defence response. There is also an issue with how cases are counted. In clinical trials, the few people who developed COVID-19 after being vaccinated may have developed a very mild version, but this is still counted as an infection. It is hard to tell right now, because these numbers are calculated on the basis of a very small sample group, usually fewer than or around 200 people. This number will be more precise when the data is based on more people and on real-life situations rather than trial settings, which is one of the reasons why the world is watching the Israel experience so carefully.
Q: The MOH advises that the approved COVID-19 vaccines are not recommended for pregnant women, severely immunocompromised persons, and children under the age of 16 years. Why is this so?
A:‘Not recommended’ does not mean that the vaccine would be harmful in any way, it is simply because these three groups of people are excluded from clinical trials. As far as we know, there is no real reason that the vaccines will harm them. ‘Not recommended’ does not mean ‘contra-indicated’. It is quite likely that within the next few months, when the results of more studies come out, these subgroups will be able to get this vaccine.
Q: Do new mutant strains pose a threat to people who have had COVID-19 or been vaccinated?
A:There are many mutant strains, but the two that are most worrying are those from South Africa and Brazil. There are some signals that even though you may have had COVID-19, you may get it one of these two strains again. There was an interesting study done in the Amazon region of Brazil. More than 70 percent of the population already had COVID-19 and therefore had antibodies, which is close to what we consider to be herd immunity. But despite that, there was a major second wave anyway. This serves as a warning that we may see new strains that have different properties, so to speak.
Q: Have there been any cases of these two worrying new strains in Singapore?
A:Not that I know of. It is unlikely that the imported cases that we are seeing come from South Africa or Brazil, due to travel restrictions.
Q: We have heard that some vaccines can alter DNA. Is there any such risk associated with the approved COVID-19 vaccines?
A:Live attenuated vaccines are made from weak live virus cells, such as measles and chickenpox vaccines. These are never given to pregnant women. However, the approved vaccines are both mRNA vaccines – or messenger RNA vaccines. These vaccines contain small pieces of genetic information that are enclosed in lipid envelopes. There are no live virus cells or DNA present, so there is no chance that the vaccines can be incorporated in our DNA.
Q: What is your general advice to the Singaporean public regarding COVID-19 vaccination?
A:The supply of vaccines is limited, and there are groups of people who will benefit more from being vaccinated than others, such as the elderly, people with serious medical conditions, and frontline healthcare workers. These priority groups will receive the vaccines first. Of course it would be nice to say – the sooner the better, but we have to balance this optimistic scenario with what is available. If and when the vaccines arrive in sufficient amounts, no doubt things will speed up. But for now, we just need to be patient, and continue to observe good hygiene, social distancing and mask wearing. That is all we can do.
Q: What are your predictions for the future of the pandemic in Singapore?
A:Locally, sooner or later, most of us will be vaccinated and our lives will slowly return to normal. In fact, it is already happening. The big question that everyone is trying to figure out is – when will the borders reopen so that we can travel again? Unfortunately that depends not only on how we handle the pandemic in Singapore, but on what happens in other countries, which is beyond our control.
Vaccines Approved for Use in Singapore
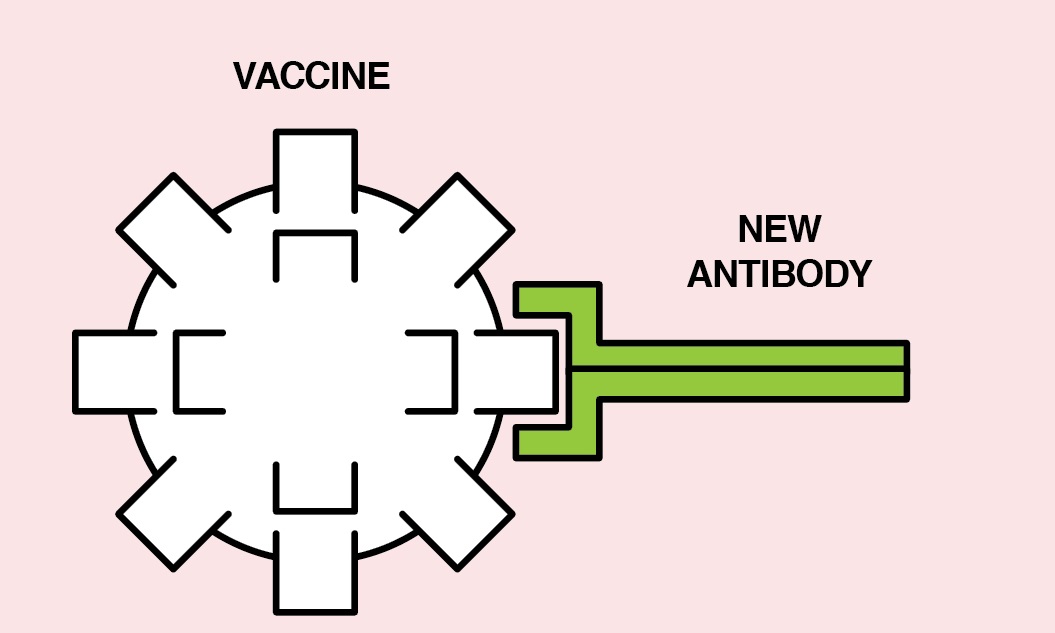
• Both Pfizer-BioNTech and Moderna vaccines are mRNA vaccines or messenger RNA vaccines
• mRNA vaccines contain material from the COVID-19 virus that gives our cells instructions on how to make a harmless protein that is unique to the virus
• Our cells make copies of the protein then destroy the genetic material from the vaccine
• Our bodies then recognise that the protein should not be there and build antibodies to fight the virus
How Vaccines Work
Human Immune System (without Vaccination)
A new pathogen or disease enters the body and introduces a new antigen. In response to the new antigen, the body builds a specific antibody. The antibody grabs onto the antigen and defeats the pathogen.
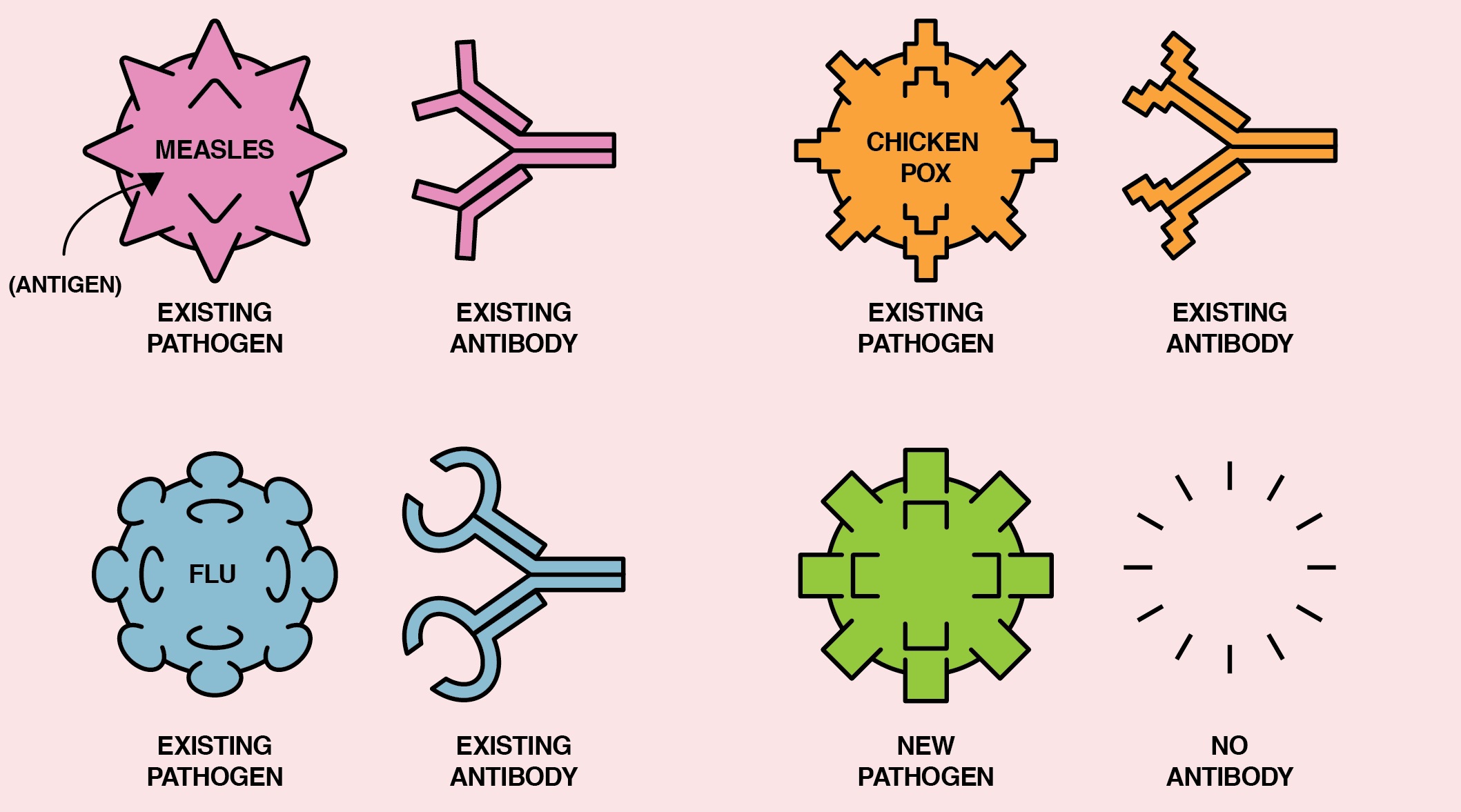
Human Immune System (with Vaccination)
A vaccine that includes parts of the antigen from the targeted pathogen enters the body.
In response to the new antigen, the body builds a specific antibody.
If the pathogen and its corresponding antigen enter the body later, the antibody grabs onto the antigen and defeats the pathogen.
SOURCES
https://www.who.int/news-room/feature-stories/detail/how-do-vaccines-work
https://www.gov.sg/article/what-you-should-know-about-the-covid-19-vaccine
https://www.reuters.com/article/us-health-coronavirusisrael-pfizer-idUSKBN2AH281
https://www.nytimes.com/2021/02/05/world/middleeast/israel-virus-vaccination.html
This article is taken from our My Alvernia Magazine Issue #44. Click here to read the issue on our website or on Magzter.