Vegan and Vegetarian Pregnancy: Ensuring Nutrient Adequacy Navigating the plant-based path to parenthood requires careful consideration of nutrient adequacy.

Parenthood is a deeply personal journey, and at Mount Alvernia Hospital, we are committed to walking alongside you every step of the way, providing expert care, compassionate support, and the essential resources you need to make this milestone truly fulfilling.
Our comprehensive maternity packages and parentcraft services—including antenatal classes, lactation guidance, and postnatal nutrition support—ensure your needs are met from pregnancy to postpartum.
Every baby is a blessing, a precious gift from heaven. As a gesture of thanksgiving, it is a Mount Alvernia Hospital’s tradition to offer a short prayer service for parents and their newborns, just before families leave the hospital. This blessing is available to all, regardless of race, nationality, or religion, and those who wish may arrange for their baby to be presented in the Quiet Room by speaking with ward staff.
We serve you and your family with love, supporting you from the earliest days of pregnancy through to the cherished arrival of your baby, ensuring that you are surrounded by compassionate care on this life-changing journey.

Recuperate in thoughtfully designed maternity wards that offer a sanctuary of comfort and privacy.
Join a maternity tour to experience the care and services that will guide you through your birth and delivery

Get informed about nutrition, stages of labor, breastfeeding, and newborn care (Parentcraft) to support your readiness for your newborn
At Mount Alvernia Hospital, our medical care is guided by a team of expert OB-GYN doctors using the latest diagnostic tools and technology. Our comprehensive approach includes a multidisciplinary team of neonatologists and anaesthesiologists, ensuring that we are equipped to handle a wide range of emergencies.
With trusted maternity nurses who bring extensive experience—backed by 5,500 baby deliveries annually—you can be confident in receiving exceptional care and support throughout your journey.

At our St Anne Mother & Child Centre, you can recuperate in thoughtfully designed maternity wards that offer a sanctuary of comfort and privacy. With our experienced team of caring doctors, nurses, nutritionists, and lactation consultants, we ensure that you feel nurtured and supported throughout your recovery.
All our maternity wards are equipped with essential amenities, including complimentary WiFi and toiletries.
Join a maternity tour to familiarise yourself with the hospital and explore the warm, caring environment that awaits you.
The 52sqm room has space to accommodate a handful of visitors comfortably.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
The 45sqm room has space to accommodate a handful of visitors comfortably.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
The 52sqm room has space to accommodate a handful of visitors comfortably.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
The 45sqm room has space to accommodate a handful of visitors comfortably.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
Our bedside meal service includes confinement meals or a selection of Chinese, Malay/Indian, and Western cuisine. Should your doctor or dietitian recommend a therapeutic diet, your meals will be tailored accordingly.
Parenthood is a deeply personal experience, and at Mount Alvernia Hospital, we are dedicated to providing you with expert advice, support, and resources to ensure this milestone is truly fulfilling.
Introducing the new St Anne Mother & Child Centre at Mount Alvernia Hospital opened in October 2023. Our maternity wards are designed for your comfort and privacy, offering essential amenities to support your recovery, post-childbirth. Designed with a blend of warmth andsophistication, the rooms offer a tranquil environment, allowing you to enjoy uninterrupted bonding time with your newborn.
From the early days of pregnancy to the joyous arrival of your baby, our comprehensive maternity care services are here to support you every step of the way. Explore our range of maternity wards and maternity packages to find the right fit for you.
Watch this video tour of St Anne Mother & Child Centre’s maternity facilities and services. We look forward to being part of your special journey into parenthood.
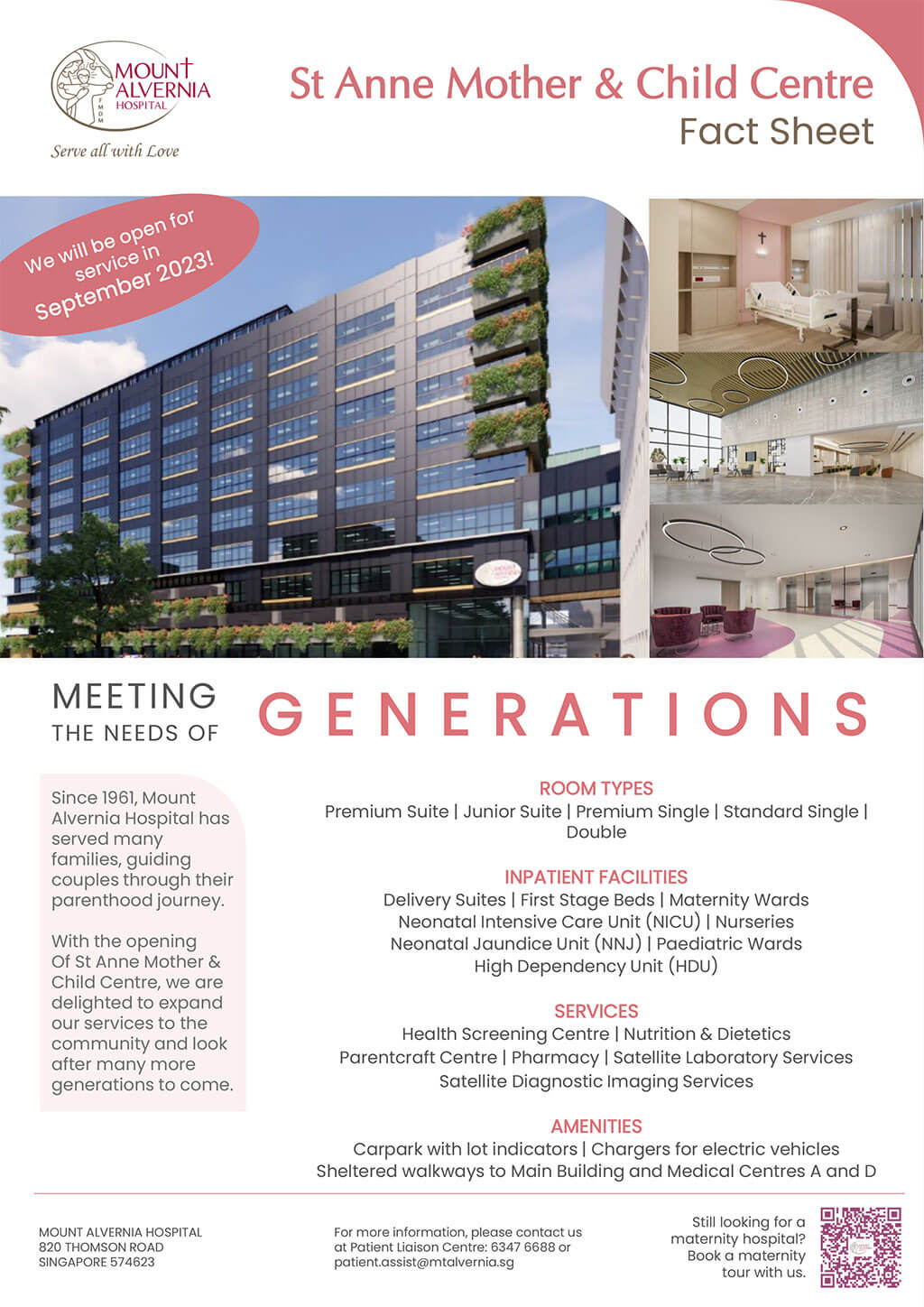
At St Anne Mother & Child Centre, our maternity wards offer comfort and privacy in thoughtfully designed spaces.
We offer different delivery options, and our experienced medical team is here to support you every step of the way, ensuring a safe and smooth birth experience.
Experience your birth in comfort, care, and confidence. Choose from four maternity packages tailored to support you and your companion.
Every mother's journey is special. Being a first-time mom or being back for your second and/or subsequent delivery again at Mount Alvernia Hospital, our maternity offerings are thoughtfully created to care, comfort, and support you so that you can focus on the joy of welcoming your little one into the world.
| Delivery Type | 2-Day Stay | |||
|---|---|---|---|---|
| Normal Delivery | Assisted Delivery | |||
| (S$) | with Epidural (S$) | (S$) | with Epidural (S$) | |
| Standard Single | 4,120.20 | 4,606.34 | 4,436.30 | 4,684.82 |
| Premium Single | 4,519.14 | 5,052.15 | 4,865.76 | 5,138.26 |
| Junior Suite | 6,587.96 | 7,390.20 | 6,767.81 | 7,434.89 |
| Premium Suite | 7,703.03 | 8,622.99 | 7,909.04 | 8,675.31 |
| Maximum Medisave Claimable (Delivery Expenses) | 3,380 | 3,650 | ||
| Additional Medisave Claimable (Prenatal Medical Expenses) | 900 | |||
Prices are effective from 15 May 2025. Prices include prevailing GST, and are subject to change without prior notice.
| Delivery Type | 3-Day Stay | |||
|---|---|---|---|---|
| C-Section | Emergency C-Section | |||
| with GA (S$) | with Epidural (S$) | with GA (S$) | with Epidural (S$) | |
| Standard Single | 6,197.74 | 6,066.94 | 9,631.24 | 9,374.00 |
| Premium Single | 6,798.33 | 6,654.45 | 9,990.94 | 9,733.70 |
| Junior Suite | 10,472.72 | 10,290.69 | 13,296.91 | 12,976.45 |
| Premium Suite | 12,300.65 | 12,089.19 | 15,387.53 | 15,019.11 |
| Maximum Medisave Claimable (Delivery Expenses) | 5,040 | |||
| Additional Medisave Claimable (Prenatal Medical Expenses) | 900 | |||
Prices are effective from 15 May 2025. Prices include prevailing GST, and are subject to change without prior notice.
| Room Type | Standard Single | Premium Single | Junior Suite | Premium Suite |
|---|---|---|---|---|
| Maternity Package | From $4,120.20 | From $4,519.14 | From $ 6,587.96 | From $ 7,703.03 |
| Daily Room Rate | $749.92 | $869.82 | $1,621.92 | $2,057.92 |
| Amenities | ||||
| TV and cable channels | ✓ | ✓ | ✓ | ✓ |
| Free wifi and local calls | ✓ | ✓ | ✓ | ✓ |
| In-room safe | ✓ | ✓ | ✓ | ✓ |
| In-room mini-fridge and beverages | ✓ | ✓ | ✓ | ✓ |
| Ensuite bathroom | ✓ | ✓ | ✓ | ✓ |
| Confinement food | ✓ | ✓ | ✓ | ✓ |
| Free Parking | ✓ | ✓ | ✓ | ✓ |
| One Adult Companion | ||||
| Accommodation | ✓ | ✓ | ✓ | ✓ |
| All meals | ✓ | ✓ | ✓ | ✓ |
| Mother & Baby | ||||
| Maternity Discharge Bag | ✓ | ✓ | ✓ | ✓ |
| Zodiac Gift Set | ✓ | ✓ | ✓ | ✓ |
| Baby | ||||
| Baby Bath Tub | ✓ | ✓ | ✓ | ✓ |
| Baby Photoshoot | ✓ | ✓ | ✓ | ✓ |
| Mother | ||||
| Inpatient Lactation Visit | 1 | 2 | 2 | 2 |
Note:
| Room Type | Standard Single | Premium Single | Junior Suite | Premium Suite |
|---|---|---|---|---|
| Maternity Package | From $4,120.20 | From $4,519.14 | From $ 6,587.96 | From $ 7,703.03 |
| Daily Room Rate | $749.92 | $782.84 | $1,459.73 | $1,852.13 |
| Welcome Back Gift Hamper | ✔ | - | - | - |
| Amenities | ||||
| TV and Cable Channels | ✔ | ✔ | ✔ | ✔ |
| Free Wifi and Local Calls | ✔ | ✔ | ✔ | ✔ |
| In-room Safe | ✔ | ✔ | ✔ | ✔ |
| In-room Mini-fridge and Beverages | ✔ | ✔ | ✔ | ✔ |
| Ensuite Bathroom | ✔ | ✔ | ✔ | ✔ |
| Confinement Food | ✔ | ✔ | ✔ | ✔ |
| Free Parking | ✓ | ✔ | ✔ | ✔ |
| One Adult Companion | ||||
| Accommodation | ✔ | ✔ | ✔ | ✔ |
| All Meals | ✔ | ✔ | ✔ | ✔ |
| Mother & Baby | ||||
| Maternity Discharge Bag | ✔ | ✔ | ✔ | ✔ |
| Zodiac Gift Set | ✔ | ✔ | ✔ | ✔ |
| Baby | ||||
| Baby Bath Tub | ✔ | ✔ | ✔ | ✔ |
| Baby Photoshoot | ✔ | ✔ | ✔ | ✔ |
| Mother | ||||
| Inpatient Lactation Visit | 1 | 1 | 2 | 2 |
| Outpatient Parentcraft Consultation | - | - | 1 | 1 |
Note:
Maternity Packages
Maternity Tours
Billing and Payments
Pregnancy is one of the most beautiful moments in life. Preparing for the birth of your child is an important journey towards parenthood.
At Mount Alvernia Hospital, we walk this journey with you to be sure that you are well supported and taken care of.
Our maternity packages are designed to provide mothers with the necessary care and comfort during this special time. With various options to choose from, you can be assured of the room type that suits your needs.
To share with you more about our maternity services, facilities and packages, we have designed the Familiarisation of Mount Alvernia Hospital’s Maternity Services which includes the Physical Maternity Tour (PMT).
This service will present what Mount Alvernia Hospital, with its years of caring for mothers and children, can offer you as the maternity hospital of choice. You can also use this session to ask our friendly hosts, the Patient Liaison Executives, any questions that you may have.
Book a Physical Maternity Tour (PMT) with us today.

Your pregnancy journey is unique and special, whether you're a first-time parent or already experienced. Let us support you through every stage—from pregnancy to post-birth care, and beyond to pediatric care for your little one.
Prenatal Care
Your journey into parenthood is a precious one, and we are here to walk alongside you with care and compassion. Regular prenatal check-ups are essential to monitor your baby’s growth and ensure both your health and your little one’s well-being.
We understand that you may have concerns about your baby’s development, and we are here to offer the support and reassurance you need. Our dedicated team of specialists will recommend any necessary screenings and diagnostics, always prioritizing your peace of mind.
If you have any concerns or need guidance along the way, you can schedule an appointment with one of our experienced obstetrics and gynecology doctors. We are here to help you and your baby every step of the way with loving care.
Here are the three stages of pregnancy you may experience:
Congratulations on your pregnancy! This exciting and crucial time comes with important steps to ensure a healthy start:
Book an Appointment with Your GynaecologistYour first visit will confirm your pregnancy via ultrasound, check the baby’s heartbeat, estimate your due date, and include initial prenatal tests.
Consider Prenatal TestingPrenatal tests monitor your baby’s development and screen for potential issues. Common tests include blood work, ultrasounds, and screenings for conditions like Down syndrome. Consult with your OB-GYN to explore your options.
Common SymptomsEach woman's experience during the first trimester varies. Symptoms like nausea, fatigue, breast soreness, and mood swings are common, with some women experiencing them more intensely than others.
You may feel a return of energy and notice your baby’s first movements as your bump becomes more visible.
Schedule Regular UltrasoundsRegular scans, including a fetal anomaly scan around 18-20 weeks, monitor your baby’s development and can reveal the baby’s gender. High-risk pregnancies may require additional tests like amniocentesis or fetal blood sampling.
Health ChecksScreen for gestational diabetes, anemia, and check antibody levels. Consider getting a flu vaccine for added protection.
Maternity Tour & Antenatal ClassesJoin a maternity tour to familiarise yourself with the hospital, and attend a childbirth education class with your partner around week 20 to prepare for delivery.
Common symptoms:Some women may experience mild cramping after physical activity, along with leg cramps, stretch marks, and skin darkening, particularly on the face and abdomen.
As your baby grows, you may experience heartburn, frequent urination, backaches, varicose veins, and hemorrhoids. Focus on health checks and preparations:
Health ChecksRegular ultrasounds monitor your baby’s growth and position. A Group B Streptococcus (GBS) screening, typically done between 35-37 weeks, checks for bacteria that may require treatment during delivery.
Increased Check-UpsExpect more frequent doctor visits to closely monitor both your and your baby’s well-being.
Physical ChangesAs your baby grows, you may experience discomforts like heartburn, backaches, and frequent urination. Your doctor can help manage these symptoms.
Postpartum SupportArrange for a confinement nanny and meal services early, and prepare any caregivers for newborn care.
Health articles to educate you through your pregnancy journey, caring for your baby, wellness and parenting your child.
Find out more education topics
Prepare for your special day with confidence—here’s everything you need to know to get ready for childbirth
Pre-register online to for a hassle-free admission process
Complete your pre-registration here before your delivery to ensure a smooth and hassle-free admission.
Hospital Bag Checklist: What to Pack for Delivery
Avoid the stress of last-minute packing by preparing your hospital bag at least 2-4 weeks ahead of your estimated delivery date.
Original Documents & Deposit
For mothers
Optional
For fathers
For baby
Plan Your Hospital Transportation
Driving yourself for delivery is not recommended. Arrange your husband, a driver or other transport arrangements to ensure smooth transportation to the hospital.
Install a Baby Car Seat
Ensure your baby’s safe journey home by installing a baby car seat in advance. You can find one at our pharmacy here.
At Mount Alvernia, our delivery wards are thoughtfully designed to provide a safe and comfortable environment for labour and birth. Located near the Operating Theatre (OT) and Neonatal Intensive Care Unit (NICU), our facilities ensure smooth and timely access to specialised care when needed, promoting the well-being of both mother and child.

To ensure a memorable and comforting experience during the birth of your baby, our delivery suites are thoughtfully designed with your well-being in mind. Each of our 15 single-bedded suites is fully equipped with modern clinical facilities and adorned in calming shades to create a peaceful environment.
We deliver around 5,000 babies every year, and our dedicated midwifery team stays up-to-date with the latest knowledge and skills through continuous education and in-house training. Rest assured that we are committed to serving you with love and care throughout the entire birthing process.
Our delivery suites are located close to operating theatres, neonatal intensive care, and high dependency units, ensuring seamless multidisciplinary care, especially in high-risk pregnancies. Your partner is encouraged to stay by your side for emotional support as you prepare to meet your little one.
Each room is equipped with foetal monitoring and baby resuscitation systems, ensuring that both you and your baby are carefully monitored at all times. Our top priority is the safety and well-being of you and your baby.
If needed, our skilled anaesthesiologists are available to provide epidural pain relief. Our caring midwives also provide one-on-one support to make your birthing experience a comfortable one.

A neonate is a newborn in their first 28 days of life and can be born either full term or prematurely (before 37 weeks of gestation). Neonatal care is a specialised field where trained professionals manage these delicate newborns.
Our Neonatal Intensive Care Unit (NICU) is dedicated to high-risk deliveries, resuscitation of sick newborns, intensive care, and well-baby nursery care, as well as follow-up. Alongside our doctors, our devoted team of nurses provides continuous monitoring, thorough investigations, and specialised medical and nursing care. We also offer comprehensive pre- and post-operative care for neonates requiring surgery.
To promote a calm environment for your newborn, we maintain optimal noise levels in the NICU using a sound level meter.

We understand that the arrival of your newborn is a precious and joyful occasion. Our Nursery Room is thoughtfully designed to provide a safe, nurturing, and serene environment for your baby during their early days.
If your baby is in good health and doesn’t need specialised medical attention, your little one can stay with you in the nurseries at St Michael, Our Lady, and St Raphael wards. Our nursery features modern facilities and is staffed by compassionate, experienced nurses who are dedicated to ensuring your baby receives the best care. We focus on creating a warm and soothing atmosphere that promotes your baby’s well-being.
Our nursery provides a supportive environment for continuous monitoring and attentive care for babies needing extra care; even for mummies requiring some recovery time, such as after a C-section.

The days after your baby’s arrival are a precious time for bonding. To cherish these moments and support you fully, we provide a complete range of postnatal services, all conveniently available in one place. This way, you can concentrate on nurturing your newborn, while we take care of the rest
After-birth care
Our dedicated lactation consultant will visit you daily in the ward, providing personalised advice and guidance on newborn care, baby bathing, and breastfeeding.
Parentcraft homecare services
Even after your discharge, our support continues. You can reach out to our Parentcraft Centre for advice and assistance as you settle into life at home with your baby. Our team is here to help you with any questions or needs you may have during this transition.
Postpartum health
We provide a range of options for weight management and exercise after childbirth. Our nutritionists are here to offer personalised guidance and support, helping you achieve your health and wellness goals with a plan tailored just for you.
Essential Products for Mother and Baby
Before leaving the hospital, be sure to visit our Alvernia pharmacy to pick up essential mother and baby products. We provide everything you need to start this new chapter with confidence and ease. And don't forget to use your Alvernia Ladies Card to enjoy exclusive discounts on our services.
Birth Registration
You can visit the LifeSG website to download the app to register your child’s birth within 42 days. After registration, you’ll receive a notification to download your child’s digital birth certificate via the Immigration and Checkpoints Authority (ICA) website.
At Mount Alvernia, we are committed to serving you and your family with love and care throughout your entire maternity experience.
Health articles to educate you through your pregnancy journey, caring for your baby, wellness and parenting your child.
Find out more education topics
Pregnancy marks the beginning of a new journey, filled with special moments of joy and challenges. Our Alvernia Ladies Card offers exclusive privileges designed to support your health and wellness. Enjoy discounts on maternity care, Alvernia parentcraft services, retail pharmacy, and more, all tailored to guide you through your pregnancy and early motherhood.
As an Alvernia Ladies Card member, you will enjoy the following benefits at Mount Alvernia Hospital:

Enjoy member rates for Ante-Natal Course, Baby Massage Course, Outpatient Lactation Consultation and Home Care Service
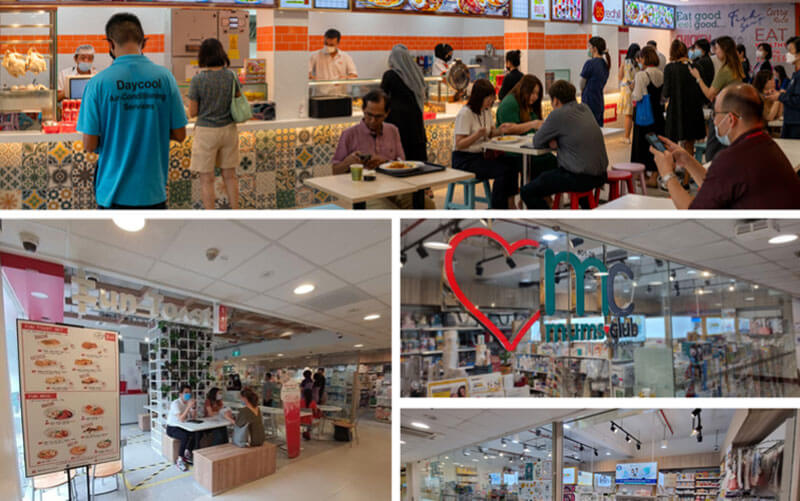
Enjoy member rates for regular priced items at Fun Toast, Mums Club, Ollella, Polar Puffs & Cakes, SF Farm Mart, SG Hawker, Subway and Umisushi

Enjoy member rates for non-medicinal products

Enjoy 12 months complimentary Singlife Family Care* coverage on accident hospitalisation benefits for mum-to-be, your newborn and your spouse
Learn more or speak to a Financial Adviser Representative at the PIAS booths or submit your enquiry via the contact details.
PIAS, a wholly owned subsidiary of Singlife has 2 booths within our hospital vicinity.

Enjoy complimentary Maternity shoot with a collage print

Enjoy special rates for Soothing Prenatal & Postnatal Massage package

Enjoy special rates for the packages below

Up to 20% Off Best Available Room (Room Only)

15% off Foundation Term (5 Lessons)

Enjoy $50 off Hegen Electric Breast Pump, exclusively at Mount Alvernia Hospital Retail Pharmacy only
Enjoy 10% off your purchase from our website (minimum spend of $50)

Complimentary Lovemère Seamless Nursing Bra

Enjoy a complimentary 1-night stay at My Queen for every 6 nights purchased. (Maximum 2 complimentary nights per stay)
10% off selected Prenatal & Family Retreat services.

Enjoy 10% off Manyue Box orders above $350 and a complimentary 4-pcs Kueh Gift Box upon successful Alvernia Ladies Card Membership registration
1 Trial Pack of New Born Tape Diapers (3pcs)
1 Travel Size Pack of Baby Safe Laundry Sheets (10sheets)
15% off all products made in www.peachybum.co (Valid for 1st purchase only)

15% off for first-time purchases made in RÓA website (1-time use per email)
5% off for subsequent purchases made in RÓA website

10% off for purchases made in SG Homemade website (Discount applicable for all items listed, including sale/discounted item/bundle)

15% off for purchases made in SLB website (One time use per member)

As new parents, it’s natural to have questions and need support ss you begin your journey with your newborn. At the Alvernia Parentcraft Centre, we’re here to walk this journey with you, offering a warm and welcoming environment designed to meet all your needs for childbirth preparation and infant care.
As an Alvernia Ladies Card member, you will enjoy the following benefits at Mount Alvernia Hospital:
Our experienced lactation consultants will share educational sessions during your stay to help you feel more confident with breastfeeding and newborn care. And because we know this journey doesn’t end at discharge, our Parentcraft Centre offers outpatient consultations, so you can reach out for support whenever you need it.
Other services include:At every step, we’re here to assist and encourage you, helping you feel empowered and cared for as you embark on this beautiful new chapter.
Childbirth Education Course (1-Day Course)
Designed by a team of experienced parentcraft specialists, this thoughtfully curated course supports new parents in their mental and physical preparation for childbirth. The course structure includes engaging lectures, informative videos, demonstrations, and hands-on practical sessions, equipping you with valuable knowledge and confidence as you transition into parenthood. We strongly encourage both you and your partner to attend together to foster a supportive and shared learning experience.
Course Topics:Labour and Delivery
Breastfeeding
The course runs from 11:30 AM to 5:00 PM, with a 1-hour lunch break from 1:00 PM to 2:00 PM. For registration, please contact the Alvernia Parentcraft Centre for specific course dates at 6347 6641.
Alvernia Ladies Card members enjoy a 10% discount on course fees.
REGISTER HEREHealth articles to educate you through your pregnancy journey, caring for your baby, wellness and parenting your child. Subscribe with us to get the latest education topics.
Find out more education topics
It is a Mount Alvernia Hospital tradition to hold a short prayer service for parents and their little ones just before they leave for home. This is to bless and give thanks for the newborn and is open to all regardless of race and beliefs. Parents who would like to have their babies presented in the Quiet Room may contact ward staff for assistance to arrange for a suitable time for the blessing.
Franciscan Blessing
May the Lord bless you and keep you
May the Lord let His face shine on you and be gracious to you
May the Lord uncover His face to you and bring you peace
Dear Valued Customer,
Please complete the form below.
Mandatory fields*